Can ADHD symptoms be alleviated by supplementing with the amino acid tyrosine? This post is a continuation from our introductory one on the effectiveness of tyrosine as an ADHD supplementation strategy.
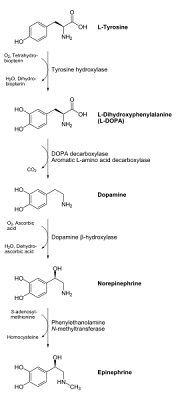
(Blogger's note: if you do not have the time or the patience to wade through all of this information, I have provided a 7-point summary at the bottom of the page, which goes over the major points of this blog posting. If you do have the time, however, there is a lot of material and valuable research in the posting below surrounding the complex metabolic processes surrounding just one step of the tyrosine supplementation pathway for ADHD treatment). The theory behind using the amino acid tyrosine to treat ADHD symptoms stems from the fact that tyrosine is a chemical precursor to important neurotransmitters (chemical signaling agents in the nervous system)
dopamine and
norepinephrine. Dopamine and norephinephrine belong to a class of signaling agents called
catecholamines. Numerous studies have shown that
imbalances of both of these catecholamine agents exist in most ADHD cases, and the imbalances are often on the low end (i.e. lower levels of dopamine and norepinephrine are found in several critical regions of an ADHD brain when compared to a "normal" brain).
Of course, this is a vast oversimplification of the whole process (which is much more complex), but the basic idea is that we "feed" the brain with higher levels of tyrosine and it is then able to create more of these two neurotransmitters. This idea, of giving the body higher amounts of starting material to use to convert into higher levels of the specific chemicals we want to produce is often referred to as
precursor loading.
Unfortunately, as we might imagine, the process of correcting these chemical shortages an imbalances (and solving all of our ADHD problems in the process) is much more complex than popping a few tyrosine supplements. Shown below is a diagram of most of the major chemical "steps" needed to go from tyrosine (written as "L-tyrosine" below) to the catecholamines dopamine and norepinephrine A larger version of the diagram can be found by clicking the figure (in most browsers, or at the original source of the diagram, which can be found
here).

We might be asking ourselves the question:
Why can't we just supplement with dopamine or norepinephrine catecholamines directly to combat these ADHD-related shortages? The answer has to do with a biochemical entity known as the
blood brain barrier.
The blood brain barrier is a special biochemical barrier used to control the transport of nutrients in and out of the brain. It is largely a protective measure, meant to keep toxic chemicals, which may have worked their way into the blood, out of the highly susceptible brain region. However, this blood brain barrier can also keep out some of our desired drug targets or chemical agents, including dopamine. Thus,
while tyrosine (or as we'll also see in a later post, L-DOPA) can cross this barrier, dopamine cannot. As a result, we need to start with either tyrosine or L-DOPA on the
outside of the blood brain barrier, shuttle these agents
into the brain, and then have the brain convert them to the desired compounds.
In today's post, we will be examining the first step of the process in more detail, the conversion of tyrosine (L-tyrosine in the diagram) to L-DOPA:

In order for this process to occur efficiently, we need three major components:
- An ample supply of tyrosine (or L-tyrosine) listed above
- A functional amount of the enzyme tyrosine hydroxylase
- Sufficient levels of a compound called Tetrahydrobiopterin.
Here's a more in-depth analysis of each of these three factors:
OPTIMIZING FACTOR #1: AN AMPLE SUPPLY OF TYROSINE:How much tyrosine is necessary to do the job?
Unfortunately, the conversion from tyrosine to L-DOPA is not a particularly efficient process. As a result, higher levels of starting material (tyrosine) are needed. Just to give a
very rough overview on the amount of tyrosine we're dealing with here in the context of ADHD treatment, typical daily supplemental doses often fall around
500 to 1500 mg per day, although there is often room for higher doses before toxicity risks set in.
At around 10-12 grams (roughly 10 times this amount), the risk of toxicity often goes way up. Other complications include high blood pressure or skin cancer (the reasons which we'll discuss in later posts), or the use of antidepressant medications, in which recommended tyrosine supplemental levels should be significantly lower (or avoided altogether).
**While tyrosine supplements can be purchased over the counter, PLEASE consult with a physician before doing any type of supplementation. In addition to the ones listed above, there are several other confounding factors which need to be taken into consideration with regards to dosing.
OPTIMIZING FACTOR #2: ADEQUATE FUNCTION OF THE ENZYME TYROSINE HYDROXYLASEKinetic studies (studies which measure the speed or rate of chemical reactions) have shown that this first step, L-tyrosine to L-DOPA is the
rate limiting step in the tyrosine to dopamine/norepinephrine process. In other words, the "bottleneck" in this conversion process lies within the enzymatic conversion of tyrosine to L-DOPA and involves the
tyrosine hydroxylase enzyme.
In addition to the fact that this enzymatic step is the slowest step in the tyrosine to dopamine conversion pathway, the
tyrosine hydroxylase enzyme has some additional challenges to overcome. One of these is inhibition by its product, L-DOPA. What does this mean?
Most enzymes or enzyme systems often have some sort of "brakes" or "control switches" too keep them from running non-stop at full speed. In other words, when the body senses that enough of the desired product is attained, it will signal for these enzymes (or other regulatory systems) to either slow down or stop, to keep things balanced and in check (think of what would happen if these feedback systems weren't in place for, say, regulating appetite and feeling full, or getting an adrenaline rush that did not subside when the perceived "threat" was over).
Tyrosine hydroxylase is one such enzyme, meaning that when large amounts of dopamine or norepinephrine are eventually produced from tyrosine, the body actually begins to shut down this enzyme-regulated conversion process. Numerous studies have shown this, as
tyrosine hydroxylase is inhibited by catecholamines.
In addition,
other enzymes also work on tyrosine hydroxylase and help turn it "on" or "off". As a result, bombarding the system with high amounts of tyrosine will not generate equally high levels of neurotransmitters, because this feedback system is in place (and we haven't even mentioned some of the potentially harmful effects of doing this, which will be discussed in later posts).
***Blogger's note: It is not my intention as a blogger to try to dazzle or confuse anyone by using all of this technical and scientific jargon. Rather, I simply want to share how much is really going on behind the scenes when we play with the levels of just one type of supplement, like tyrosine. Having said this, I personally feel that a lot of false hope is created by advocates of supplement treatment for ADHD, as these proponents often over-simply these complexities and exaggerate the overall efficacy of these "natural" ADHD treatments. I personally would like to see more non-medication treatments tried out for ADHD management, but it is a disservice to anyone if these non-drug treatment options for ADHD aren't addressed with a similar level of scrutiny.Getting back to the topic at hand...
Further clouding the
tyrosine hydroxylase enzyme issue is the fact that there are several different forms of this enzyme which exist across the population. The enzyme
tyrosine hydroxylase is actually coded for by a gene on the
11th human chromosome, which goes by the same name, the
tyrosine hydroxylase gene.
It is important to note that slightly different versions of this gene among the human population actually result in slightly different versions of the tyrosine hydroxylase enzyme. A growing body of evidence suggests that individuals with certain genetic variations of this
tyrosine hydroxylase enzyme are more
prone to certain psychiatric disorders. While it appears that ADHD is not as strongly connected to this gene and enzyme as other disorders (such as schizophrenia or Parkinson's), it is important to note that ADHD
does share some degree of biochemical overlap with some of the disorders mentioned.
It is important to note that this
tyrosine hydroxylase enzyme does not act in isolation. As mentioned in the previous post, many enzymes require special "helping" agents called
co-factors, which are needed to help stabilize the enzyme or system of enzymes and influence their chemical functionality.
Many vitamins and minerals serve as co-factors for various enzymes. In the case of
tyrosine hydroxylase, a major necessary nutrient co-factor is iron. As we will see later, iron has all sorts of implications with regards to the dopamine synthesis pathway. This has effects on both ADHD, as well as common comorbid (co-occurring) disorders to ADHD, including sleep disorders such as
Restless Legs Syndrome. In other words, it is imperative that adequate dietary intake of iron in necessary to provide the body with enough of this vital nutrient to allow enzymes such as
tyrosine hydroxylase function properly.
The
tyrosine hydroxylase enzyme is bound to iron. You may remember from high school or college chemistry classes that iron typically exists in two major form, the
ferrous form (a "+2" positive charge) or a
ferric form (a "+3" positive charge). It turns out that these two forms of iron actually exhibit major effects on the function of this
tyrosine hydroxylase enzyme.
Blogger's note: The following explanation will contain a fair amount of chemistry jargon. If you have any sort of science background, you might find it interesting, if not, please skim the next few paragraphs, and we'll meet up at the bottom where I summarize these findings and applications of this info:
As mentioned above, ferrous iron is
the less positively charged (or, in chemical terms, less "oxidized") form of iron, while ferric is the more positively charged or more oxidized version of iron. Both of these forms can be embedded in the
tyrosine hydroxylase enzyme. It turns out, however, that it is the less-oxidized
ferrous form of the iron (+2) that is required for the enzyme to convert tyrosine to L-DOPA.
On the flipside, the more oxidized
ferric form of the iron (+3 charge) is actually the form of the enzyme which plays a major role in
shutting down the enzyme's production by catecholamines, as in the process of feedback inhibition mentioned above.
Overgeneralizing and oversimplifying a bit here, it is advantageous for our system to keep this iron in the
tyrosine hydroxylase state at the
less-oxidized ferrous form if we want to keep the enzyme running (again, this is a gross oversimplification, but the general idea holds).
If you've been reading this blog for awhile, you may have come across a post a few weeks ago entitled
10 Ways Vitamin C helps treat ADHD symptoms. In this posting, we discussed some of the interactions between vitamin C and iron, and how the vitamin can not only aid in the absorption of iron (thus helping to boost iron levels necessary for proper enzyme function) but also to act as an antioxidant on the iron.
Branching off of this idea, maintaining the necessary antioxidant pools via vitamin C or other antioxidants (which will be discussed shortly), we can help keep the iron in the tyrosine hydroxylase enzyme in the reduced ferrous state and aid in the tyrosine to dopamine conversion pathway. Some earlier mammalian studies have found that activity of the
tyrosine hydroxylase enzyme is compromised in a state of severe vitamin C deficiency (scurvy), with the probable culprit being the inability to maintain the reduced (+2) ferrous state.
In other words, vitamin C can influence ferrous iron levels, which then influences the tyrosine hydroxylase enzyme.
OPTIMIZING FACTOR #3: THE NEED FOR TETRAHYDROBIOPTERIN (and cofactors necessary for the regeneration of this tetrahydrobiopterin)We have seen that vitamin C can help stabilize the
tyrosine hydroxylase enzyme. However, the main factor in regular tyrosine to dopamine conversion stems from a compound known as
tetrahydrobiopterin, which is often abbreviated as
BH4. Tetrahydrobiopterin (along with molecular oxygen) is a major cofactor of the
tyrosine hydroxylase enzyme, and responsible for the addition of the hydroxyl (-OH) group to the tyrosine molecule to produce L-DOPA.
This compound is manufactured in the human body, so (except in the case of rare genetic or metabolic disorders) supplementation with tetrahydrobiopterin or its chemical precursors is not necessary. However, its synthesis (from its own series of enzymes) is dependent on adequate levels of nutrient
cofactors including magnesium and zinc. Prolonged deficiencies in either or both of these minerals can therefore potentially inhibit the synthesis of tetrahydrobiopterin, and, indirectly, the tyrosine to dopamine conversion process. Please note that we have discussed both
magnesium and
zinc in great detail with regards to the roles they play in the onset and treatment of ADHD.
In addition to the indirect relationship between tetrahydrobiopterin and ADHD due to the impact on dopamine synthesis, tetrahydrobiopterin is important in numerous other functions as well. For example, low levels of tetrahydrobiopterin in the body have been associated with
hypertension and other types of cardiovascular dysfunction.
If tetrahydrobiopterin (BH4) is the predominant compound for the tyrosine hydroxylase enzyme function, is vitamin C still potentially useful in the process?While BH4 is a more powerful regulator of the
tyrosine hydroxylase enzyme in the tyrosine to L-DOPA ADHD treatment pathway, there is some evidence that vitamin C can "help the helper". A much older study, done way back in the 1970's suggests the benefits of
vitamin C on the synthesis of catecholamines like dopamine and norepinephrine. The reason given in this article is the role of vitamin C in recycling or regenerating functional forms of the tetrahydrobiopterin compound.
The whole concept of vitamin C recycling other nutrients is not new to this blog and its discussions. We have mentioned how
vitamin C can "recycle" other antioxidants such as vitamin E, and how this can have an indirect impact on nutritional treatment strategies for ADHD.
To summarize the key points and suggestions which should be taken away from this the blog post:- Do not overdose on Tyrosine supplementation. For reference, a ballpark estimate on dosing is often somewhere around 500 to 1500 mg per day, but please do not start any type of supplementation without consulting with a physician.
- Tyrosine hydroxylase is the key enzyme in the conversion of tyrosine to L-DOPA. It is contains iron which must be kept in the reduced (+2) state to function properly. Naturally, this means that the enzyme can be compromised if an iron deficiency is present. Recommended daily intake levels for iron can be found here.
- It is believed that this tyrosine hydroxylase enzyme can be aided by maintaining ample levels of antioxidants such as vitamin C in the diet. Keeping antioxidant levels up to speed aids in maintaining this necessary form of the iron for the enzyme to function properly. In other words, the enzyme is intricately connected to antioxidant balances in the body. This is an often overlooked side-component of ADHD treatment via tyrosine supplementation. here is a link for the recommended daily intake for vitamin C.
- Tyrosine hydroxylase is inhibited by its own products, the catecholamines (which include dopamine and norepinephrine, two of our later "targets" in the above diagrammed pathways). This means that we cannot expect to get high levels of dopamine in the brain by mega-supplementing with tyrosine, because this process shuts itself off.
- Therefore, excessive tyrosine supplementation (beyond the level recommended by your physician) is essentially ineffective, and potentially harmful.
- The main helper of the tyrosine hydroxylase enzyme, however, is the compound tetrahyrobiopterin. This is manufactured in the body, so supplementation for this is not necessary (except in the case of a few rarel genetic or metabolic disorders). Tetrahydrobiopterin and molecular oxygen (O2) supply the enzyme with the proper tools to convert the tyrosine to L-DOPA by chemically adding a hydroxyl (-OH) group, which can be seen in the diagrams near the top of the post.
- Tetrahydrobiopterin synthesis is dependent on nutrient cofactors including zinc and magnesium. Recommended daily amounts can be found here for zinc and here for magnesium.
In our next post, we will be looking at the second major step of the conversion process from the tyrosine to dopamine pathway. This will rely heavily on enzymes known as decarboxylases. We will be looking at how these enzymes work, what nutrients (or co-factors) they need, and examine to see if there are any interfering factors or side-effects involved, as a way to optimize this process of tyrosine supplementation as an ADHD treatment strategy.